Weaving the Thread of Social Services into Community Health
- aspenideashealth

- Apr 21, 2020
- 6 min read
Updated: Nov 16, 2020
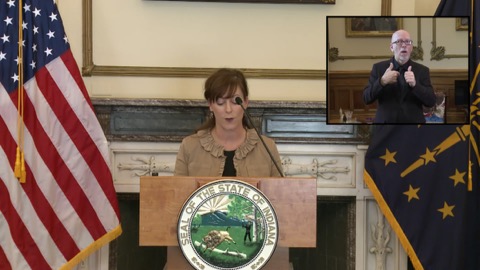
As the Secretary of Indiana's Family and Social Services Administration, an emergency room physician, and a public health expert, Jennifer Sullivan shares her perspectives on state-based responses to the COVID-19 pandemic, the role of social services in community health, and innovation in health care delivery.

Let’s start with the topic on everyone’s mind: #COVID19. You are board certified in emergency medicine and have a degree in public health. And, of course, you hold a very senior health position in the Governor Eric Holcomb's cabinet. Knowing the many hats you wear, we'd like to get your perspective on the current situation and its impact on the people you serve.
What are you experiencing in Indiana and how has the state approached its response to the outbreak?
Indiana has taken a very scientific approach to our COVID response and I have been very proud to be a part of that. We have a large group of clinicians across multiple state agencies that have really come together to help our Governor make public health decisions that will (and have) saved lives. We also have a data team that helps us understand what is happening in real time (where, what, who). This helps not only in decision-making but also in communication with the public why we are doing what we are doing.
We have been incredibly lucky that the collaboration across public, private and nonprofit sector has been amazing. Our hospital systems are collaborating at the regional level, for example, to share people, equipment and surge space capacity. We also wove social services supports into our response from the beginning so that SNAP, Medicaid, TANF, and Childcare could be supportive throughout tough policy changes like "stay at home" orders.
We have seen a heartbreaking number of deaths despite these efforts and hope that our interventions will help those plateau very quickly.
As an emergency room doctor, what is it like to be on the frontline of the pandemic?
The main reason that I’ve remained in practice during my entire time as a public servant is to make sure that I can understand, in a tangible way, the needs of my patients and the needs of the health care system as “one of them.” This time is really no different. I can see and feel the stress in our trainees, in our nursing staff, in my colleagues and I can also see the incredible leadership in our health care systems to prepare for surge and protect people. At the same time I can talk to patients and families about their unmet needs (food, housing, childcare, etc.) and take their voices back to my work at the state level.
Working on the front line makes me incredibly proud to be part of a group that continually runs to the fire. We will never close our doors, we will always take care of the people who need us.
As a public health professional, what should Americans take away from this experience in terms of better understanding the focus and goals of public health?
Public health never gets the credit for what doesn’t happen, only the blame for what does. The infrastructure for public health preparedness is critical for the present and the future. As we move into recovery (hopefully soon!), we need to bolster this infrastructure and make sure that training this critical workforce is a priority for the future.
As Secretary of Indiana’s Family and Social Services Administration (FSSA), how have your priorities shifted in response to the pandemic? Have you seen states coming together to develop a regional approach?
I am really fortunate to have an incredible leadership team at FSSA and made my deputy the acting secretary at the beginning of our response so that I could focus solely on COVID and the critical work of our agency would still have a steady hand and great leadership. Our agency leadership team is focused on making access to health care coverage, as well as social services, as easy as possible. This includes tele-health and tele-psychiatry access. I believe we issued a record number of Medicaid bulletins last week (April 12-18) – 28 at last count – to make sure that Hoosiers are getting what they need. Despite these temporary changes, we remain committed to our mission, vision, and values to improve the health of Hoosiers.
Our focus on social determinants of health runs as a thread through our entire COVID response.
I don’t think that anyone has the corner market on good ideas and sharing those across state lines to help protect people from second waves of surge is a great plan. We certainly have taken that approach here in the Midwest.
Balancing your duties and responsibilities, what keeps you up most at night during this pandemic? The tough ethical decisions that come up if we truly hit “phase IV” surge where we don’t have enough resources to provide high quality care to patients keeps me up at night the most. I know in my head that I’m not solely responsible for that, but in my heart I won’t be able to rest until we have exhausted every possible angle and resource to keep people safe.
There is a Mary Oliver poem with a line “Was I right, was I wrong, will I be forgiven, can I do better?” that plays in my head constantly.
Also, the mental health and psychological ramifications of what we are asking people to do weighs heavily on me. Since I have mental health and addiction in my agency’s portfolio, we have been able to actively work on that throughout, but are seeing the untoward effects of isolation in increased suicide hotline calls, incidents of domestic violence, and the anxiety that comes with economic uncertainty. How we handle that for the long recovery ahead is paramount.
Major crises, like the COVID-19 pandemic, have a way of shining a spotlight on societal gaps that already exist. For example, racial disparities that have been well documented in our health care system long before COVID-19 are on full display right now. How might we turn the current spotlight on health disparities into an opportunity for change? We knew the gaps in Indiana’s health outcomes that pre-dated this pandemic would be even more exposed than they were before. Addressing these health disparities is a top priority for health care, public health, and social services. The OB Navigator project that launched in 2019, for example, is based on blending what we know works in health care and public health to improve infant and maternal mortality, this being a key priority of Governor Holcomb. The program utilizes a community-level social determinants of health approach for groups who continue to have disproportionately poor outcomes. Our black infant mortality rate is starting to improve because of this approach. In addition to health disparity, we know we have to address health inequity, which is harder to talk about because it means that health disparities are happening because our systems have design flaws that cause harm. This is the inherent, and often not recognized, bias that happens in our communities, our socioeconomic structure and even in the halls of medicine that places minority populations at greater risk for poor outcomes than disease qualities would predict alone. Indiana’s data suggests that we are no different than other states experiencing these issues with the novel coronavirus pandemic. This is an ongoing problem that will only be mitigated by 1) acknowledgment 2) partnership for understanding 3) changing our structure to recognize bias before harm occurs 4) active outreach for groups who have been systematically marginalized and 5) comprehensive understanding of the needs of individuals/families who we are asking to do these difficult strategies like social distancing.
Because of this spotlight, we have an opportunity to change at an individual and a system level to make a rapid series of improvements. We will not let that opportunity pass us by.
We know that much innovation in health and health care delivery often originates at the state level. Perhaps the best example of innovation coming from the state of Indiana is HIP – the Healthy Indiana Plan -- which, in essence, replaced Indiana’s traditional Medicaid program for able-bodied adults. What prompted the change in structure? How do you measure “success” in terms of the changes have been made? The Holcomb Administration has been fortunate to do two rounds of HIP renewal to enhance the innovations for Medicaid expansion that began in 2010. One that I’m most proud of is our pending Bridge application that will allow individuals transitioning to marketplace or employer insurance to take their health savings accounts (we call them POWER accounts) with them to cover gaps in premium payments, medications, co-pays, etc. to help mitigate the “cliff effect” that happens with a rapid but often small change in income. HIP has a great history, starting under then Governor Mitch Daniels, as a way to provide coverage for individuals above the eligibility level for Medicaid. This was done as a block grant through tobacco tax funds and covered about 40,000 people a year. Under the Affordable Care Act (ACA), we expanded HIP and now are able to cover 400,000 Hoosiers to help improve health outcomes across Indiana. The HIP model has worked for Indiana because of incredible partnerships and we have seen improvements in health outcomes and a larger ability to recruit health care providers to accept Medicaid. We have a long way to go, but this has been a great first step.
The views and opinions of the author are her own and do not necessarily reflect those of The Aspen Institute.













Comments